Peripheral Spondyloarthritis
Reviewed by: HU Medical Review Board | Last reviewed: October 2022
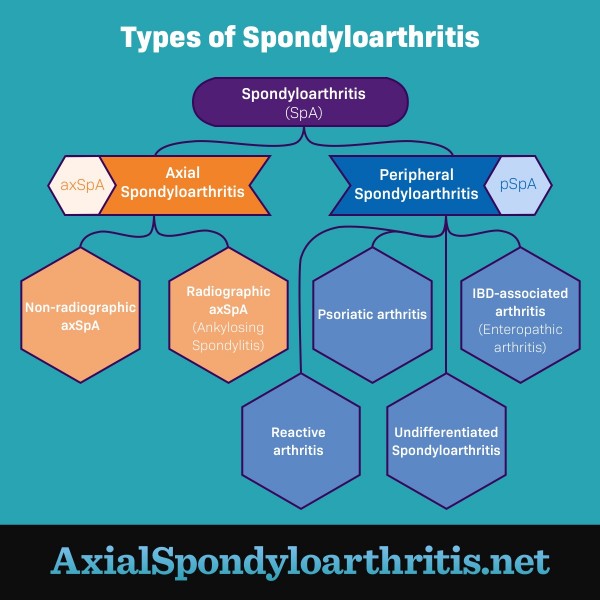
Spondyloarthritis is a type of arthritis that affects the joints and the areas where ligaments or tendons attach to bone. There are 2 main types of spondyloarthritis: axial spondyloarthritis (axSpA) and peripheral spondyloarthritis (pSpA).1
AxSpA symptoms typically occur in the spine. People whose symptoms occur in places other than the spine are diagnosed with pSpA.1,2
Types of peripheral spondyloarthritis
There are several types of pSpA. They include:1,2
- Psoriatic arthritis (PsA)
- Reactive arthritis
- Arthritis with inflammatory bowel disease (IBD)
- Undifferentiated spondyloarthritis
- Juvenile spondyloarthritis (JSpA)
Figure 1. The different types of spondyloarthritis
Psoriatic arthritis
PsA is a chronic condition that causes pain, swelling, and inflammation in the joints and tendons. Most people with PsA also have psoriasis, a skin condition that causes red, scaly patches.1,3
The most common areas of the body affected by PsA are:1
- Hands
- Feet
- Wrists
- Knees
- Ankles
Some people with PsA also have one or more "sausage digits," toes or fingers that swell between and around the joints. This is also called dactylitis. Also, some people with PsA have pain and stiffness in the spine.3
About 1 to 2 people in 1,000 have PsA. The condition impacts all genders equally. Up to 30 percent of people with psoriasis also have PsA.3
Reactive arthritis
Reactive arthritis is an uncommon condition that can occur when you get an infection in another part of your body. This infection most commonly occurs in the urinary tract, gut, or genitals.4
Most people with reactive arthritis have symptoms that come and go, including pain and swelling in the joints. Symptoms usually go away completely within 12 months.4
Arthritis with IBD
One type of arthritis, called enteropathic arthritis (EnA), is fairly common in people with IBD. About 1 in 5 people with IBD develop EnA. Doctors think EnA results from the immune system mistaking healthy cells for harmful ones. EnA mostly affects the joints in the arms and legs, but it can develop anywhere in the body.5,6
Undifferentiated spondyloarthritis
Undifferentiated spondyloarthritis is diagnosed when a person does not meet the exact criteria for another type of spondyloarthritis. Your doctor may use the term "unclassified spondyloarthritis" to refer to this condition as well.7
Juvenile spondyloarthritis
Arthritis conditions that begin before the age of 16 are called juvenile spondyloarthritis. These conditions can be either peripheral or axial. Their severity varies from child to child. Treatment is often similar to that of adults.8
How is it diagnosed?
PSpA is diagnosed through a detailed physical exam by your doctor. Your doctor will use several factors for diagnosis, such as:2
- Your symptoms, including the location of your joint pain, type of swelling, and other clues like a classic rash
- Features of specific conditions, like a psoriasis rash or bowel problems with IBD
- Other conditions that could cause joint pain
Because there is no one-size-fits-all way to diagnose pSpA, your doctor may need to perform other tests to reach a diagnosis.2
Featured Forum
View all responsesHow is it treated?
Depending on your condition, you may need to visit different specialists for treatment. Goals of pSpA treatment include:9
- Reducing pain and inflammation
- Slowing or stopping joint damage
- Improving physical function
- Preventing sudden, severe symptoms (flares)
Treatment may combine prescription drugs and other methods. Drug treatment might include:9
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen. These drugs decrease inflammation. They are available over the counter or by prescription. They are often the first-line drugs used to treat pSpA.
- Disease-modifying antirheumatic drugs (DMARDs), such as methotrexate. These drugs decrease pain and inflammation. They also aim to slow the progression of pSpA.
- Biologic DMARDs, such as etanercept or adalimumab. These drugs work by blocking a specific protein (TNF). They may help stop your symptoms, depending on your condition.
Preventive and non-drug treatment options might include:9
- Exercise, stretching, and physical therapy
- Achieving and maintaining a healthy body weight
- Stopping smoking
- Maintaining a healthy diet
There are many ways to treat pSpA, and understanding your options will help you make the best decision for your care. Work with your doctor to develop a treatment plan that is right for you.