Adapting To the Disappearance Of Restful Sleep
It feels like common knowledge that the right amount of sleep can help with productivity, brain functioning, and maybe even help you live longer. However, for those of us with inflammatory conditions like ankylosing spondylitis (aka axial spondyloarthritis), getting enough sleep - and restful sleep at that - can feel out of reach.
I had a history of sleeping well
Sleep was no problem for me as a child and teenager. I slept soundly, even with 130 mile per hour winds from hurricanes battering the tin roof of my childhood home on the coast of North Carolina. In college, back spasms began affecting my ability to fall asleep, though I did sleep soundly after falling asleep.
While awake, however, I was a fidgety kid. I could never sit still, always jiggling a leg, stretching my arms, or doubling myself over my knees to pop my back. I began running 5k road races when I was seven; I juggled multiple sports in middle and high school, and I played soccer for a Division 3 college. My identity was 100% athlete: I was always moving when I was awake.
My diagnosis brought new realizations
After my AS diagnosis in 2013, four years after graduating college and at least 13 years from the time my symptoms began, I realized in hindsight that my childhood fidgeting was to prevent pain that was always lurking beneath the surface.
I also discovered that, as my AS worsened, sleep became more difficult.
At best, AS is effectively managed with a good mix of medication, diet, and exercise; and, at worst, its severity can cause spinal fusion and systemic complications. No matter which outcome, we with AS endure chronic pain that is worse than anyone should ever have to accept. Including when we're asleep.
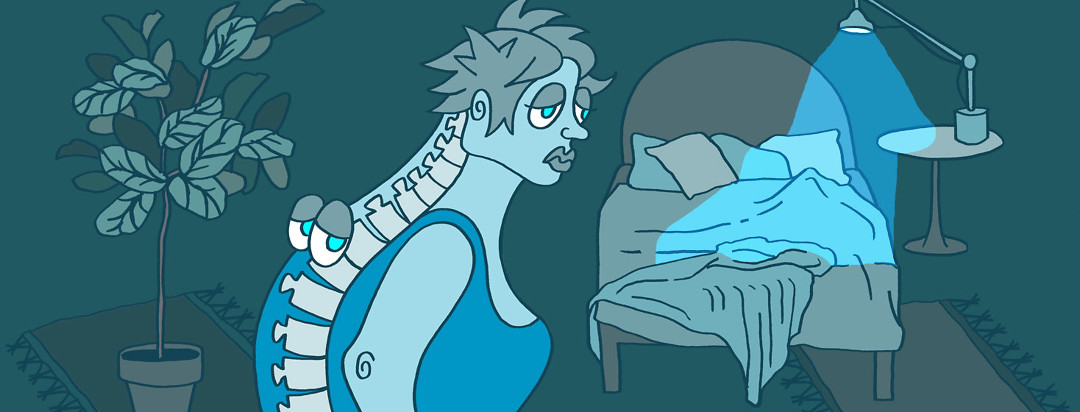
Sleep for people with AS isn't restful
During sleep, it's generally a given that joints rest, bodies heal, brains digest. But with AS, when our bodies rest we become stiff and sore. The most restorative thing there is - or should be - can be destructive for us. Ironically, sleep can be exhausting for us.
We need sleep, we want sleep, we are desperate for sleep. But sleep often hurts us, begetting the phenomenon of, as Dawn Gibson identifies as "painsomnia."
AS bodies defy a big rule we've been taught about life: rest feels nice.
Finding the balance is near impossible
In reality, our bodies exist in competition with themselves. There's a tiny window where everything is perfect; we've moved enough that we're no longer stiff, and we haven't moved so much that we've crossed the threshold into the dangerous territory of Over-Doing-It-ness. Often, we don't know when we're overdoing it until after it's already happened.
Balancing on this thin wire constantly, enough that it becomes subconscious - a constant withholding and fear of our own bodies paired with hope for activity we can't sustain - is exhausting. The key is finding the middle ground between rest and movement without overdoing it, but even that is a challenge because that "middle ground" moves every day.
Sleep, for us, is a brief rest from our bodies' constant hunt for that elusive middle ground; but beneath the surface sleep also presents as a danger, threatening damaged joints as a byproduct of inflammation at rest. After my diagnosis in 2013, no matter what I tried to do to get restful sleep, my body begged to differ. I eventually learned to stop expecting that a night of sleep would be a refreshing reset.
I've tried it all
Like others with chronic diseases, depression and anxiety also affect my sleep. It took a long time for me to seek professional help; I had tried everything from herbal remedies to meditation to shutting my phone in another room at night. Nope, nothing helped. It wasn't until I found the right mix of medications prescribed by both my psychiatrist and rheumatologist that I found out exactly how much sleep I was really missing.
On top of using medication for pain and mental illness, I also developed a set of home-hacks for sleeping. Note that none of this should be taken as medical advice.
Sleep hacks:
- I see a therapist weekly
- I use a weighted blanket
- I sleep on a heated mattress pad and in the winter I add a heated blanket on top of everything to make a heat-sandwich
- I take my evening medications at the same time each night
- If I can't sleep or when I wake up in the night, I have my phone nearby to read or I ask my smart home device to play a meditation. Even if I can't sleep, I treat resting opportunities like sleep
- I try not to schedule activities first thing in the morning
- I no longer blame myself for not being able to sleep. I allow my disease to take responsibility for that. I also accept that it is my disease that needs care rather than blame, and that it is only with constant communication with my body, and accepting help, that I improve
Accepting ankylosing spondylitis and insomnia is key
I have learned that taking advantage of any tool that can help me do more with my body - including sleep - is the exact opposite of shame. It's empowering - a reclaiming of part of my life that I get to live on my own terms.
I still don't get the sleep I used to, and I don't expect it will ever be great, but after accepting help with sleep, my quality of life has improved noticeably. The thing is, I know I'm going to have to adapt for the rest of my life when it comes to managing any aspect of living with AS.
And I'm learning to be ok with that.
Community Poll
What topics are you interested in learning more about?
Join the conversation